I suffered from mental illness for 37 years.
I have never been mentally ill.
My wife worked hard at school. She was keen to please her parents and teachers. Because she was good at her work she was pushed to be even better. But she was pushed too hard. As a result, shortly after the beginning of her second term at college, she suffered a nervous breakdown. She had to give up her course. From then on she had to scale down her efforts. She took a lesser course closer to home. Apart from a couple of minor relapses, her illness seemed to be all but over, an unfortunate one-time occurrence.
A Disruptive Illness
We got married in 1967. We moved into our first home. It was a small cottage in a small village close to where I worked. My wife was going to start a career teaching cookery. But this never happened. She had a couple of small unexpected relapses. Then, immediately after our daughter was born, she developed what was diagnosed as paranoid schizophrenia.
From then on, for the next 10 years, she had full relapses every 2 to 3 years. Each relapse lasted between 3 and 6 months. The illness is traumatic. One who has never been mentally ill can have no idea what it is like. One who has never lived with a mentally ill spouse can have no perception of the effect it has on family. How then can clinicians and administrators presume to judge our needs and decide what help we shall, and shall not, be given?
I have never been mentally ill so I cannot know directly what it is like for her. I can only attempt a sincere speculation based on my observations and listening to what she has said about it. So here goes.
Imagine that you are living your life and going about your daily tasks as normal. The relationships you have with those around you are pleasant and stable. You are happy.
Suddenly, you realise that those around you — those whom you trust and depend on, those in official positions, those with whom you have to deal in shops and businesses, those you pass the time of day with — are all starting to change. They are starting to talk subversively about you behind your back. They are starting to plot against you. Their acts of apparent service and kindness to you are covertly laced with ulterior motives which you cannot quite discern.
Whereas they once made passive comments or even paid complements, now they insult you and throw offensive retorts. Your whole life and wellbeing is under threat. All your relationships become steadily more confrontational and aggressive. You become frightened and confused.
You perceive the world's response to your presence as aggressive and threatening. You defend yourself. You meet perceived aggression with real aggression. The world responds to your real aggression with real aggression. And so it escalates in a super-regenerative loop until the white van arrives and you are forcibly constrained and removed to a locked cell in a mental hospital. Drugs are forced into you. You know not why. The world takes on an even more threatening form. You then endure weeks of hell until the drugs have dulled your mind sufficiently to make the rest of the world perceive you as harmless once again.
It is like an irregular cycle of seasons. The world — your social environment — is basking in a warm gentle summer. Then, slowly but resolutely, the seasons change. The tranquillity of your summer world falls through the turmoil of a tempestuous autumn into the cold confusion of winter. Hospital treatment then conveys you through an emerging springtime of recovery until you are released into a new summer of normality.
Distorted Perception
When you are finally released back into the community, you find it hard to believe that you were ever ill. As you see it, you have been normal all the time. You did not sense the changes in yourself because the part of you that changed was the very means with which you measure change.
In fact, the world did not change at all. Due to a chemical imbalance in your brain caused by a slight malfunction in a simple gland, the 'lens of perception', through which your mind brings your sociological world into focus, had become distorted. So the world as you saw it was not the world as it really was.
But this mental lens of perception is the only conduit through which you can experience reality. Therefore you have no absolute frame of reference against which to compare your view of the world in order to be able to see that it is distorted. To you, what you see is your frame of reference. You have no means of knowing that it is you who are ill.
Seen As A Lesser Person
Although all may now see you as strange, most try to be understanding. Despite this, among your friends and your extended family, you discover that you're somehow — by default — regarded as a less significant person. You are not at the forefront any more. You are expected to take much more of a back seat now. Your opinion no longer has quite the same weight.
To control your condition you now require a monthly injection of drugs. These keep you on an even keel, but they also slow you down considerably. You cannot work at anything like the pace you would need to do to hold a job. But you soldier on. You work hard to keep up with your housework, shopping and family washing.
A Commendable Achievement
If you lose a leg you lose mobility. Lose a hand and you lose dexterity. But if you lose your mind you lose yourself. You lose who you are and what you are. You lose your identity. You lose your self-respect. You lose the respect of others. You lose benefits of formerly acquired skills. You lose the status of prior academic achievements.
Before her illness, my wife was every bit as dynamic and capable as her sisters. In fact, academically she rose to far greater heights. Battling against a recurring mental illness while succeeding at running a home and bringing up children is at least as meritorious as holding down a powerful position in business. Rebuilding confidence and repairing relationships after a relapse takes courage second to none. It demands a sustained determination. Of all things, it is worthy of the utmost respect.
Effect on Family
My wife's condition does not only affect her. It also affects her family, her neighbours and anybody else with whom she may have contact.
Long-term or permanent illness of any kind — physical or mental — is an enormous burden on any family. I have heard of and read many articles about this kind of burden, to which the State pays nothing but a glancing lip service. The most recent case that springs to mind is that of a gentleman called Peter Lodge. He was the full-time carer of his son David, who was autistic and had learning disability, dyspraxia and other complications.
NOTE: I too am autistic, with an Autism Quotient of 44 on the Cambridge Autism Research scale. And I'm the carer, not the patient. My case, however, is on a very different part of the 'spectrum' from David in that I have what used to be called Asperger's syndrome.
From the article, it came across to me that Peter was David's officially-recognised carer, whereas for the whole 37 years during which I cared for my wife and family, I had no official recognition whatsoever as the carer of my schizophrenic wife with her entitlement personality disorder, plus my daughter and two sons. I was required to be in permanent full-time work and was chastised and passively punished for being physically and mentally unable to fulfil this requirement.
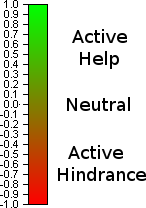
I do not mean in any way to belittle Peter's gargantuan difficulties. Nevertheless, this meant that, whereas Peter received at least some miserable financial pittance as a carer from the penny-pinching British State, I received nothing, being made to live under the constant threat of destitution. I imagine that Peter at least received a sympathetic attitude from society and authority, whereas I received disapproval, contempt, active hindrance and being labelled as a good-for-nothing layabout that didn't think he ought to contribute to society. This is the result when the quacks can't see what they are looking at and won't even condescend to admit that there is a permanent burdensome condition.
NOTE: a quack is someone who professes knowledge that he does not have. These medics, for the most part, didn't have the necessary knowledge to enable them to diagnose my wife's blindingly obvious condition at these critical times. Consequently, my use above of the word quack is entirely appropriate. Notwithstanding, in the context of my wife's condition, I think it should be seen as applying to the entire profession rather than just to the individual medics involved. They may understand how to set broken bones. But regarding my wife's [somewhat unusual] condition, they know nothing.
On top of all this, a patient with a physical illness is invariably co-operative with family and medical professionals. They understand that they are ill and want to get better. They can be reasoned with.
My wife, on the other hand, because her illness is mental, never co-operates with family or medics because she does not realise or accept that she is ill. Her perception of the world and other people is distorted. She thinks in a way which is disturbingly strange to people who are not mentally ill. Consequently she does irrational things. Not necessarily harmful. Rarely a physical 'danger to herself or others'. Rarely if ever criminal. But far more disruptive to the day-to-day lives and tasks of those around her.
For example, once when my wife was approaching full relapse, all our vital documents disappeared — birth certificates, insurance policies, medical cards, tax returns, mortgage documents and also cash. My wife said she had stored them in safe places to protect them from burglars. After she had gone into hospital, I discovered one of these quite by chance. It was an insurance policy. It fell out of an old newspaper I took from a pile in the shed. I was about to light a fire with it to burn some rubbish in the garden. Safe from burglars it certainly was. Who would ever think of looking in such a place for valuables? But safe? Certainly not. It could have been thrown out or burned at any time. I then had to search every nook and cranny in the house to find the rest of what had disappeared. That took a long time.
Another example is a distorted sense of value. Waste not, want not is my wife's perfectly reasonable philosophy. It is also mine. The problem is that free-market capitalism is based on waste. You have to throw things away. That is how it works. But to my wife in a relapsing state of mind, things like empty packets and plastic bags became just as precious as things like furniture, carpets and curtains. We had to keep and store them all indefinitely. They may come in useful one day. The result was that once, just after she had been taken into hospital, I had to have a fire in our empty concrete coal bunker which I fed continuously with rubbish for three days. I really mean I was stoking it continuously. The house up until that point was completely constipated. It could not function as a home.
But by far the most difficult thing I have had to wrestle with in these circumstances is what I call the hidden agenda. We have all come across the career climber. He gives the appearance of working wholeheartedly for the team, the project or the company, while relentlessly pursuing a hidden agenda for personal betterment at the expense of his colleagues — often badmouthing them to higher management in order to get himself ahead. I always found these people easy to spot. Like most of their colleagues, I could see through their hidden agendas. This is because their hidden agendas follow a rational straight-forward route and is fuelled by the simple motive of selfish gain.
Not so easy with the hidden agenda of a schizophrenic. All throughout each approach to relapse, my wife knew full well that others thought she was ill. But she wanted to avoid the inevitable. For this she devised a hidden agenda for getting away from the inevitable consequence. But her agenda was not rational. It followed a very convoluted path. Its goal was not even rational.
One time my wife piled lots of our valuables into the back of our car and drove off. I did not know where she was going. An hour or so later she arrived home on foot. She had parked the car somewhere with lots of our valuables visible in the back. She would not say where she had parked it. It was in a safe place, she said. I asked the police if they could find it. They searched but could not find our car anywhere. Days later, I eventually found it parked behind a bound load of bricks on a building site. Safe place for a car full of valuables? I don't think so. After she came out of hospital, she told me that she had been planning to escape to some friends about 250km away in Yorkshire. Those friends had, however, since moved to Germany, so they would not have been there anyway.
All this manifests itself as a tremendous extra workload and level of stress upon me and our children. Yet we must still soldier on with our jobs, studies and other obligations of normal living. For the full duration of each relapse this is an on-going and relentless war of attrition. The collateral effects of mental illness on carers and family is something with which medical professionals, social services and society in general are coldly unconcerned. Their exclusive concern is for the patient.
A Permanent Problem
Relatives, friends, neighbours and professionals see, and partially appreciate, the trauma which this mental illness precipitates upon our immediate family during a relapse. However, they all seem to embrace a universal and unfounded assumption that once my wife is out of relapse, everything is back to 'normal'. It is not.
The permanent symptoms of her entitlement personality disorder remain. Once out of relapse my wife thinks and acts in her normal way. This normality is maintained by a monthly injection of anti-psychotic medication. This reduces her mental speed and organising ability. This in turn reduces her capacity for work. As a result she is far slower than most people in accomplishing ordinary day-to-day tasks.
She is far too incapacitated for permanent employment. She tried to get work after her first two or three relapses, but each time she was quickly sacked for low productivity. Her illness has made it difficult for her to retain procedural knowledge. So despite her obvious intelligence and prior academic achievements, she is essentially unemployable outside the home. Consequently, I am my family's only possible 'bread-winner', even though the 24/7 coverage necessary in the 6 month run-up to relapse leaves me little or no time to win bread — a situation which is intransigently unrecognised either by the medical profession or social services.
Besides her injections of medication, my wife needs something else in order to remain stable and active. That is the constant presence of somebody close who understands the nature of her illness. Namely me. This is evinced by the diagnosis entered on her application for Disability Living Allowance in 1999 by the psychiatrist, who attended her as an outpatient:
"A SCHIZOPHRENIC ILLNESS
She is unemployable and needs the supervision of the psychiatric team. She is on a care programme with approach planning. She needs the supervision of her husband."
If she were left on her own for too long, a small concern would rapidly and irreversibly escalate into a crisis. Preventing such a crisis demands no time or effort on my part except to be there. For all practical purposes that means 24 hours a day, 7 days a week.
Until the point is reached at which a doctor and a social worker together have certified my wife, the children and I have had to endure the symptoms of the illness alone.
Unpredictable bouts of irrational behaviour. Twenty-four hour a day hyper-activity. Endless telephone calls to others — family, friends, my employer — about what an evil, abusive, nasty person I am. The disruption of every household process. Complaints from neighbours. Exposure of our property to loss and theft. Potential financial ruin resulting from large irrational expenditures by somebody who is still at that point legally sane and responsible. The most notable of these during the two months or so before relapse is the telephone bill. My wife is on the phone to anybody and everybody all day every day. Even if you have a teenage daughter, believe me, you have no idea what a telephone bill is — especially if, unlike me, you have never had to make ends meet from this miserly misnomer called welfare.
The approach to relapse is not smooth or linear. My wife does not gradually get more and more ill. In the early stages, she is raving and irrational for an odd half hour. Then she is perfectly normal for two or three days. Over the following weeks, the periods of disruptive irrationality increase in intensity and duration until they eventually merge into a continuous condition.
During that time, she seems to be able to control her episodes of disruptive irrationality to some extent. She may delay them or bring them forward to suit her agenda. And guess what? Every time she has a scheduled visit to the psychiatrist or is visited at home by a community psychiatric nurse [CPN], she is always on her best behaviour. In fact, her disposition in the presence of a medical professional (or indeed any other 'outsider') seems to exhibit a disturbing element of almost psychopathic coolness. She may be mentally ill but she is not stupid. She is in fact highly intelligent and adept — certainly sufficiently so to fool a psychiatrist or a CPN. This should be no surprise. Neither of them has more than fleeting contact with her. A half hour interview per month — or even per week — is nowhere near a sufficiently high sampling rate to facilitate the detection of such a sporadic phenomenon.
During a typical on-set of relapse, my wife's paranoid episodes follow a pattern like that shown below.
The paranoid episodes are represented by the intermittent 'square wave' pulses. Outside the bounds of these disruptive periods she is her normal self. She isn't even a bit paranoid. Her illness is undetectable.
The changes between her paranoid episodes and normality are like when switching the channel on a television. On one channel is football: on another channel is a film. When you are switched to the football channel there is no trace or evidence of what is taking place in the film. When you are on the film channel you are unaware of what may be happening in the football game. Events in the film are not influenced by the football game on the other channel. The outcome of the football game is in no way determined by the story unfolding in the film.
The station transmitting the football and the station transmitting the film are operating independently and concurrently. The one you see at any given time is simply the one to which your receiver is currently switched. I sense that likewise, both the 'normality' channel and the 'paranoid' channel are transmitting concurrently in my wife's brain and that the one you see at any given time is simply the one to which her consciousness is currently 'switched'. I am no professional, but that is the way it seems to me. To my wife, on the other hand, her periods of paranoia and normality seem to form a perfectly rational continuum. She sees nothing abnormal as having taken place throughout.
If I call the doctor or the CPN during a severe paranoid episode, then by the time the doctor or CPN arrives, the episode is over. She has switched channels. The medical professional declares that there is nothing wrong with her. I am made once again to look a complete idiot or a scheming husband who wants to put his wife away so he can 'make whoopee with another woman' or something. I am given the chastising look as if to reprimand me for wasting their precious time.
I cannot imagine any other branch of science or engineering attaching any credibility to such a cack-handed observational method for monitoring such a sporadic condition. Of course, my observations as one who is with her 24 hours a day apparently carry no credibility whatsoever. The medics seem to take absolutely no notice of what I say, except to attend what they see as yet another false alarm from an incompetent layman.
From the accumulated proportion of time my wife is in a disturbed state, one could calculate the probability of a doctor or CPN by chance interviewing her during one of these episodes. I have no quantified observational data, but intuition strongly suggests that the true likelihood of her being caught is well below this computable probability. This is because I think she can exert a high degree of control over when an episode actually occurs. This is helped by the fact that no interviews ever occur at night or at weekends. Consequently, for a very long time indeed, our children and I are the only ones who witness — and suffer — any of her paranoid episodes.
My intuition is that these sporadic episodes form something resembling a temporal Cantor set. I sense that the chaotic switch which triggers these episodes carries on operating all the time irrespective of medication. We who live with her see the first half of the cluster leading up to full relapse. The episodes in the trailing decline, after she has been admitted to hospital and is on heavy medication, are still there but their external effect is so much attenuated by the medication as not to be noticeable. I suspect that if she went through the whole process without medication then the episodes would gradually subside on their own in about the same time it took them to reach their crescendo.
A Heavy Burden
This makes life exceedingly difficult for me. During such a time my wife watches me like a hawk. I cannot use the telephone. I cannot leave the house without a legitimate excuse. And I cannot fool her. She is far too perceptive for that. She can see through just about any motive or intent. Eventually I slip through enemy lines and manage to contact a CPN. The CPN reluctantly arranges an unscheduled home visit. Guess what? When the CPN comes, my wife is on her best behaviour again. I end up looking a complete idiot, or possibly a fussy intolerant husband who wants to get rid of his wife by having her committed to the loony bin. Instead of being nipped in the bud, this gives the illness time to grow and intensify until eventually she has to be taken into hospital forcibly 'under Section'.
Seeing her taken in under a Section of the Mental Health Act is not a pretty sight. I remember one time after weeks of stress that finally the ambulance and the police came. My wife did not want to go. They decided the only way was to force her into the ambulance under restraint. After vain attempts to negotiate with her, the doctor and social worker gave the ambulance men the go-ahead to carry her into the ambulance. They could not get hold of her. She went into a corner of our living room and would not move. The two policemen who had come along assisted. The two ambulance men took one of her arms and the two policemen took the other. I turned round to leave the room thinking that it was at last all over. Then I heard an almighty crash. I turned back around to see my wife alone in the corner where she had taken refuge. The four big burly men were in a heap 7 metres away in the diagonally opposite corner of our living room. I don't think they even knew what day it was.
When in a disturbed state my wife is exceedingly strong. I don't know the medical reason. Perhaps in that state her blood stream contains an unnaturally high level of adrenaline. I eventually persuaded her that going into hospital was the only reasonable thing to do. But consider for a moment the stress of living with a disturbed person who is many times your strength, but whom society regards as the poor weaker vessel. If she becomes disturbed in a public place, the bystander always assumes that I am the culprit. They give me the disapproving eye. If they intervene they side with her until they become totally confused. Then they normally go away, leaving an exacerbated situation.
The Discredited Carer
We are all a mixture of good and evil. We all have virtues. We all have faults. Some have more virtues than faults. Others have more faults than virtues. But generally, within each of us, each fault and virtue has a relative dominance or recession such as to allow us to function reasonably within society at large.
In order to function within society, one has to relate with others. To be able to relate safely with others, one needs to be able to know how much one can safely trust each other person with whom one relates. This requires the one to examine and classify the faults and virtues of the other. The shape and form of this classification gives rise to one's view of the other's character. The truth of this view depends on the accuracy with which one perceives the relative strengths of the other's faults and virtues. Though never perfect, it is generally supposed that one's perception of another's faults and virtues is sufficiently linear to render a fair picture of what kind of person they are, so when one speaks honestly of the other to a third person, the report is fair and true.
During the on-set of relapse, my wife's perception becomes increasingly distorted. She therefore perceives some faults and virtues in a particular person as vastly stronger or weaker than they actually are relative to all their other faults and virtues. It is as if she is looking at the page of one's mind, over part of which is placed a small very powerful magnifying glass. And the glass invariably falls over a part of the page describing a fault. Consequently, while in a relapsing state, when she speaks honestly of another person to a third person, the report is anything but fair and true.
The person with whom she has most to do in life is me, her husband. So when in a relapsing state, what she relates to others about me is nothing short of total character assassination. She will wax thunderously for hours about my evil deeds and intents against her. Such an evil deed can often be something which happened deep in the distant past (25 years ago or more). It is blown up out of all proportion to its context and spoken of as if it happened yesterday. The result is that all her friends — and indeed a lot of other people besides — rapidly come to regard me as an extremely bad person.
This has happened every time my wife has relapsed over the past 33 years. One particular incident springs to mind. I took her to her chapel in Hertford. That chapel has since closed. It is a strict sect. I do not share their beliefs, nor do I feel comfortable among the people. I did not attend the event. I simply took my wife there, waited in our car during the service and took her home again afterwards. When the people came out, one who was some kind of visiting minister came over to the car and spoke to me in a very irate manner. He then launched into me and gave me 'a thoroughly good talking to' about how I ought to be ashamed of myself about the despicable way I treated my wife. I looked him straight in the face throughout his 'admonition' and said nothing. There was no point. I had no idea what he was talking about. I still have no idea.
Being discredited to her religious 'friends' is of no real consequence. However, during the on-set of relapse, my wife has also said great and terrible things about me to relatives. My mother told me that my wife had once shouted all manner of defamatory things about me to her down the telephone. It greatly upset my mother. Eventually, my mother said to her, "Well why don't you divorce him then? You would certainly have my blessing!" My parents are both convinced that divorce would be by far the better state in which to spend what is left of my life. They are undoubtedly right.
What is a Carer?
I have discussed the plight and difficulties I have caring for my wife. But I have not yet discussed what a carer actually is. I only came across the term recently (summer 2000) when my GP suggested that I could possibly benefit from attending a newly formed Carer's Group which met at the local mental health support unit. I attended the meetings until my wife became too paranoid about my being influenced by the other carers of mentally ill relatives.
The events of my wife's last relapse however soon made it quite clear that the title of 'carer' is an empty and toothless title. A carer has responsibility but no power. This was demonstrated by a particular event. My wife had been in a state of relapse for some weeks. In the CPN's professional judgement, however, there was nothing wrong with her. She was just angry. The CPN's team leader was contacted by my wife's sister. Between them they decided that what my wife needed was to get away from home somewhere and away from me.
As a result, my wife's other sister pulled rank over me as her carer and took my wife 130 km away to Kent where they would care for her. Both when she arrived and when she left with my wife, I told her sister that she was taking my wife from me out of my care against my expressed wish and better judgement. She took no notice. Four days later, the sisters had decided that my wife was ill as I had said. They called the doctor. The presence of the doctor caused my wife to demand to be taken home. Their local doctor injected her with a heavy dose of temazepam so that her sister could drive her back to me as soon as possible, having thoroughly exacerbated the whole problem.
It seems that as her carer, I have no authority to tell interfering relatives what they may or may not do regarding my wife when she is not in a state fit to make her own decisions. Responsibility without authority is a complete and unworkable nonsense.
The Time of Trouble
The pre-relapse phase can go on for a long time, especially since doctors are very reluctant indeed to respond to a request by somebody else to attend a person who strongly denies that they need treatment. This is because the doctor-patient relationship is regarded as private, personal and confidential — even from relatives. The patient's 'rights' must be upheld. This may be an appropriate policy for people with physical illnesses who are of sound mind. However, it is entirely out of place with mental illness. The stress and disruption caused by the illness to others — including children — makes it their business too. But their 'rights' and well-being are ignored.
Consequently, during the approach to, and throughout, each relapse I have, under these circumstances, had to:
- maintain a full-time level of income
- run and maintain my household
- take care of my children outside school hours
And I have had to do all these things concurrently and single-handedly.
Without my full-time income I could not have paid my mortgage on top of meeting my household costs and the extensive travel costs of visiting my wife in mental hospitals, some of which have been over 150km away from my home. My income has never been high enough to enable me to buy domestic help or child minding services. There is therefore nobody with whom to share the load or to allow me time off for a break.
After each relapse when my wife returns home from hospital she needs a lot of attention. She needs a lot of bed rest. She needs feeding. She needs clean clothes. She cannot do anything but relax and recover from her treatment. So in addition to my already excessive workload I then have to be a full-time mental nurse also.
On-going
Gradually, upon returning home from hospital after a relapse, my wife would become able to do things. She would start to make meals. Then she would take on the washing and shopping. But even when she is officially 'fully recovered' these three take up her full week. Whenever she takes on an extra project, such as gardening or painting a picture, one or more of these three chores gets left undone.
I have to clean the house, the dishes, transport my wife to wherever she needs to go for shopping on the market or to hospital appointments. And 'earn' my living at the same time. The reality was that after a full week's work I had to spend all weekend clearing up and cleaning the house and carrying on with whatever house maintenance project was currently on the go. There was never time to rest.
In the early years I simply soldiered on alone with these things. However, I was a lot younger then. I had what now seems to me to have been an inexhaustible supply of physical energy. I could not do it now.
No Help
During the early stages of a relapse, family, friends and neighbours are quick and willing to help. But this help rapidly evaporates after about a fortnight. They then realise that they have their own lives to carry on with. Their own chores have mounted up. They have no more time. Furthermore, their help is limited to shopping, washing and child minding. Assisting in the handling of somebody approaching relapse is beyond them. I could not reasonably expect family to be able to take too much of the load. They all live much too far away. This is because I had to move to where I could find work (as one is inevitably forced to do in a capitalist free-market economy).
Naively, I had expected society to help. All my childhood teachings about helping those in need and all the Biblical sentiments with which my young mind had been indoctrinated in those far-off days led me to assume that it would. But it didn't. It has increasingly become far more concerned with appeasing the greedy voting tax-payer by allowing him to keep more and more of his so-called 'earnings', leaving less and less for helping those in need. As a result, apart from 2 hours a week of domestic help for a very short period immediately following my wife's return home from hospital sometimes, there has never been any source of on-going help from the instruments of the State — financial or otherwise.
The apparent policy of Social Services is that, for the duration of my wife's relapses, I should continue in my permanent job and that our child should be taken into official 'care'. This very nearly happened. But my wife had heard from others in the same predicament that once a child is taken into 'care' it is all but impossible ever to get the child back. To me this idea was anathema. I had to find another way.
The final permanent employer I had was very understanding about my wife's illness. Nevertheless, as with family, friends and neighbours, there is a soon-reached upper limit to what employers are prepared to forego. After all, they are competing in a marketplace with other companies who do not have to support employees who need an indeterminate amount of time off at unpredictable times.
There is also the problem of active disruption to business. During the approach of relapse, I would go to work as usual each day. Then as soon as I got there the telephone calls would start. Call after call after call. No sooner would I get her off the phone than she would be calling again. I remember one time when she was being particularly 'persistent'. The telephonists downed tools, refusing to answer calls. The switchboard of a multinational company was grid-locked by one woman. I certainly could do no work. I don't think many others could either.
Permanent Job Impractical
The problem came to a final head when my wife had a sudden relapse while I was in Antwerp. I was about to attend a briefing with technical staff at a Belgian multinational. My sister-in-law telephoned my hotel with an urgent message that my wife was very ill. Apparently my wife had made a disturbingly irrational phone call to her sister. It had seemed so desperate that she went (or was taken, I do not know which) 130km to her family's farm. In the telephone call to me her sister said that I had to return home immediately because they could not cope with the situation. I excused myself from the meeting and caught the next aircraft home. When I arrived at my wife's family's farm I found that my wife had been admitted to a local mental hospital. This was 150km from our own home. It seemed that the crisis was over and that it had been completely unnecessary for me to waste the expensive time of my employer's customer's technical staff by withdrawing from the meeting they had convened to brief me with information.
This was far from the first time I had had to leave work urgently in such circumstances. Often I was left with no option but to bring my young daughter to work with me. The women members of staff were especially helpful and gave her little inter-office errands to keep her entertained. But this situation could not go on. It became increasingly clear that it would soon become impossible for me to do my job. There was no possibility of progressing my career further. Even with the high capacity for work I had in those younger days, I could only be in one place at one time — at home or at work. Clearly I needed to be in both. The only practical solution was for me to work at home.
Becoming Home-Based
Being able to work at home would solve the problem completely. I would be there for when my daughter came home from school, was off sick from school or on holiday. I would be there when my wife returned from hospital and thereafter. All I needed was a source of work. The nature of my work did not require a large factory, heavy plant or expensive equipment. Initially it required only a desk, a typewriter and a telephone.
In the wake of the great advances in telecommunications technology during the 1980s and 1990s, many of the major telecommunications companies have been featured in articles and television documentaries on home-based working. They call it teleworking or telecommuting. The executives of such firms enthuse at great length about it. They encourage their customers to establish tele-workforces. However, they themselves seem most reluctant to practice what they preach. Whenever I approach such firms, I am told that they are not interested in my working for them on that basis. It seems that the privilege of teleworking is reserved for long-established 'trusted' executives and women who do remotely monitored piece-work in data entry and word processing. During my intense search over 10 years I have found no permanent jobs for which the employer will allow the employee to tele-work from home.
My only option was to become self-employed, finding my own work piece by piece from the open market. This I did one way and another for 15 years. However, my family circumstances meant that I was in effect working with one hand tied behind my back so to speak. I was competing with people who did not have the same constraints imposed upon them. The income I made from self-employment never approached the salary of a permanent job. Nevertheless I regard that 15 years as successful. This is because during my years in permanent jobs my wife was ill on average every 2 to 2½ years. Since I became self-employed in 1976, she has been ill only twice, and on each occasion the integrity of our family unit was preserved without disruption.
Official Attitude
The clinical professionals in charge of treating my wife's illness obviously understand something of the physiology of her illness, though they still seem unsure of what to call it. Some call it schizophrenia, others say she is 'schizo-effective'. Furthermore, their concern is strictly limited to the physical and psychological well-being of their patient. They have no apparent interest in the social dimension of her illness, namely, the effect it has on her immediate family and others. It seems that this is outside their professional brief. In fact, it does not seem to be within anybody's professional brief. Consequently, as far as officialdom is concerned, my wife's illness does not in any way disadvantage me in the process of trying to 'earn my living', so-called. As far as the State is concerned I do not have a problem, and therefore need no help or concessions.
My wife's friends and relatives are the same. They see the poverty resulting from my being unemployed as the problem. "With his skills, why doesn't he get off his butt and get himself a job? It's a disgrace." They do not have to look far for the answer. But they cannot be bothered to look. They do not want to see. Society offers no recognition, help or thanks to one who cares for a mentally ill relative. Only condemnation.
Professionals have vast knowledge about the mechanics of the illness. They know all about transmitters and inhibitors in neural synapses. They know which drugs and what quantities of them attenuate the symptoms of the illness to the appropriate degree. They have heard many patients describe in words their feelings and perceptions which result from the illness. But they themselves have never experienced the illness. The words spoken by the patients are just symbols. The listening professional has no real frame of reference within his mind against which to perceive truly what the patient is describing.
Furthermore, the professional is with the patient only occasionally for short sessions in the artificial environment of his consulting room. He has no experience of what it is like to live and cope with the patient 24 hours a day without a break within an ordinary home with its inadequate medical and human resources. So as regards the sociological aspects of the illness too, the professional is no more than an observing theorist. This is probably why the professionals — and consequently the welfare officials they advise — have no conception of the hardship such an illness places upon a patient's family. This is evinced by the structure and content of the idiot tick-box forms through which they expect us to be able to 'communicate' our needs to them.
 Their blindness to this hardship would be excusable but for one thing; namely, that there is a source of insight into the fact that this hardship exists. That source is the patient's family. What is inexcusable is that this source is ignored or, at best, regarded as having insignificant credibility. The result is the continued non-recognition of this hardship. But sadly, official non-recognition does not make the problem go away. I wish it did. If this professional non-recognition merely resulted in a neutral situation in which the patient's family received no help during a relapse, this would at least be survivable. But it does not. On the contrary, it has created active hindrance to my efforts to contain the disruption.
Their blindness to this hardship would be excusable but for one thing; namely, that there is a source of insight into the fact that this hardship exists. That source is the patient's family. What is inexcusable is that this source is ignored or, at best, regarded as having insignificant credibility. The result is the continued non-recognition of this hardship. But sadly, official non-recognition does not make the problem go away. I wish it did. If this professional non-recognition merely resulted in a neutral situation in which the patient's family received no help during a relapse, this would at least be survivable. But it does not. On the contrary, it has created active hindrance to my efforts to contain the disruption.
Problem With The Law
As with many things, the one thing which amplifies and exacerbates the myriad difficulties of mental illness is our all-invasive asinine English law. It seems that a doctor is allowed to base a recommendation that a patient be forced onto medication only on what he himself directly observes of that patient. This is probably why they declare my wife well if she is so during their interview with her — no matter what trauma, disruption or hardship her activities may have caused to the children and me over the previous days, weeks or months.
It seems that the only thing with which the Law is concerned is whether or not the patient is perceived by the examining doctor to be a danger to herself or to others. I think there is a serious problem with the definition of the word 'danger' and each professional's interpretation of the word 'danger'. I don't think my wife would ever intend to harm anybody. Nevertheless, her amplified strength when in a disturbed state is potentially dangerous. I feel distinct pain on my kidneys and rib cage when she hugs me aggressively when ill. And she did throw two policemen and two ambulance men across our living room. But this is not the point. To my mind there are other forms of danger.
Providentially it did not happen, but if my wife's last relapse had started 3 months earlier it would have been at its most disruptive right in the middle of my younger son's A-level examinations. Despite his being predicted high grades (which in the event, he achieved), he would not have stood the slightest chance of passing a single examination. Being kept awake all night by shouting tirades, he wouldn't have had a prayer. In that state, my wife is wholly unconcerned with, and oblivious to, any consequences of what she is doing. Yet the Law does not class this as 'a danger' to others. It would certainly have been a danger to his future career, income and well-being — especially after the two years of extremely hard work he had put into his learning. Being on welfare, we certainly could not afford to keep him while he took his examinations again.
My younger son went on to university. But my elder son lived with us through my wife's last relapse. He could not sleep. He could not do his job properly. He had to turn away the driving instructor and forfeit the cost of 4 hours worth of driving lessons because he was too exhausted on his day off to drive. My wife's tirades drove him from our home twice. He first stayed with his sister and then with friends. Yet the Law says she is not 'a danger' to others. I think that in a materialist money-driven capitalist society like ours, being driven to the point of not being able to work, without any officially acceptable excuse, definitely is dangerous.
The upshot is that my wife's immediate family — her husband and children — have to endure months of intolerable abuse from her before society will trouble itself to intervene. Even then it intervenes only for the 'good' of the patient: not for the health, safety or sanity of her family. As her family, we have to suffer this abuse for two months or more. For example, during our brief respites of glorious sleep in the depth of the night we are repeatedly hammered back into consciousness by being relentlessly shaken and shouted at. This alone would be internationally condemned as torture if it were perpetrated by the interrogators of a Draconian regime. But under English law it is perfectly acceptable for a relapsing schizophrenic to perpetrate it upon her husband and children for weeks and weeks on end. Of course, while all this is going on, that same society expects me to provide evidence each fortnight that I have been 'actively seeking work every day' and for my son to provide his employer with a good full day's work.
Society requires that the patient's rights be protected at all costs. And what costs they are. But it provides the members of the patient's family with no practically enforceable rights whatsoever. As in almost everything, I think that in this too the Law needs seriously to examine itself. It is time those irresponsible guffawing buffoons who exchange their idle banter in that little hot air parlour by the Thames were given a taste of what they inflict upon others by their incompetent and callous stupidity.
If the Law allowed a patient to be forced onto medication at the first signs of relapse then neither the patient nor the patient's spouse and children would be subjected to this recurring two months or more of unmitigated hell. The only person qualified to decide if and when the first sign of relapse has occurred is the one who is able to observe the patient 24 hours a day 7 days a week. And that person can only be the patient's legally empowered carer. A caring spouse who has lived with the patient through over 30 years of this unbearable illness I think has thereby demonstrated above anybody in the world that he has the patient's interest at heart. He serves out of love alone. He has no financial reward, only the financial loss of having to exist on the miserly national disgrace called welfare. No paid professional could possibly have this dedication, qualification or reputation. And it is about time it was said.
An Impossible Position
My wife is a loved and valued person. I am not a clinically aloof professional. I am her husband. I am emotionally involved. She has been the prime source of inspiration and encouragement which has kept me going throughout my life. Seeing her ill is very painful for me. She is intelligent, artistic and academic. She is currently writing a book giving her own account of her illness. To the casual observer we are a normal happy family.
But 30 years experience of this illness have shown me that if I were to take a normal job which took me away from home from nine-till-five every day, then my wife would quickly relapse — professional opinion notwithstanding. The solution could be so simple were it not for the bloody-minded inflexibility of employers and the blind forces of the so-called 'free' market.
As a result I am now in an impossible position. I have no capital of my own with which I could re-start my business independently. I spent all my capital trying vainly to keep going during the recession of the early 1990s. I am also ineligible for any State business start-up initiatives because I was self-employed before becoming unemployed. Besides, I have no 'redundancy' money to put up as the mandatory capital contribution to the available business start-up schemes. I am therefore required by law actively to seek full-time permanent employment — and provide evidence each fortnight that I have indeed been so doing — or lose my only source of life-support, namely the lowest possible level of State welfare.
My adopted policy is, with best endeavour, to seek a permanent full-time job, shutting my mind to the consequences unless and until I am offered one. Then I shall be forced by society to make the final decision on which to sacrifice: my wife's sanity or our measly income. A society which perpetrates such callous injustice and unnecessary suffering does not itself deserve to prosper or even survive.
As for my personal life, due to the disruptive nature of my wife's illness and her paranoia — exacerbated by our long-term financial poverty — I have not been able to socialise or have friends. And though I am — and have always been — physically fit and healthy, the intense psychological stress rendered me sexually impotent from 1985 when I was only 43, since which time I have had to suffer the added undertow of a completely arid existence.
The Final Straw
After my wife's seventh relapse in the year 2000 [on top of my son's first relapse in February 2000 and his second relapse in December 2000, which was undoubtedly exacerbated by the sleep deprivation he suffered as a result of my wife's relapse] I found myself gradually collapsing under the strain. I soon discovered that it was no longer just a matter of 'pulling myself together' and renewing my resolve as in the past. I was no longer merely suffering temporary exhaustion. This time it was permanent debilitation.
As reluctant as I was to accept this, I realised that, at the age of 58, I could not foresee myself dealing with future relapses into my old age. My physical and mental resources were spent. I could no longer envisage a future of trying to contain and survive my wife's behaviour while fighting the negative pressures placed upon me by society through arrogant medical professionals and intransigent Social Service bureaucracies.
Over the next 3 years, my emotions went into free-fall. It was as if my conscious mind were living day to day while, unbeknown to it, my subconscious mind was covertly searching for a way of escape. Having been on welfare for over 10 years, and therefore having no financial resources whatsoever, the practicality of escape seemed impossible.
Some Pivotal Advice
Then, by chance, I met a certain medical professional, who wasn't directly involved, and who allowed his conscience to get the better of his medical ethics. He warned me that if I didn't find a new life for myself, I wouldn't last much longer. He said that while I was there, Social Services would do nothing. But if I disappeared then my wife would be at least looked after. I knew he was right.
This medic related the case of another patient, who was cared for by his brother. His brother died. He was literally worked to death. But the patient had no posthumous thanks or appreciation for his brother. He simply continued criticising and condemning him for not being there any more [to serve him].
Medical ethics require that a medical professional respect his patient's confidence and act always and exclusively in his patient's best interest. Notwithstanding, if to do so effectively aids and abets the flagrant and inhumane violation of another person's fundamental human rights, then conscience requires the medic to act otherwise. That natural conscience should take precedence over artificial medical ethics is self-evident.
Having to continuously contain my wife's very difficult behaviour renders me permanently stressed and deprived of sleep thereby making it impossible for me to have a permanent job or even run a home-business. The medics are wholly incapable of recognising symptoms or even seeing that there is anything wrong at all. As a result, the DSS regards me as an undeserving "good-for-nothing layabout who doesn't think he ought to contribute to society". Hence we are left to precariously 'survive' on the lowest level of so-called 'benefit'. This significantly jeopardises our children's education because they are the school paupers who can't afford the extra books and activities in which their peers participate.
I assert that this be a deliberately enforced violation by the British State of my and my children's self-evident human rights, especially Article 22 of the Universal Declaration of Human Rights of 10 December 1948.
This medic's parting comment to me, as if throwing me a lifeline, was: "Your wife is bad as well as mad". I never saw him again.
However, his comment fired me into action to find out what my wife had been saying about me so freely behind my back for the past 37 years to friends, family, church, DSS officials and NHS staff. So I did something illegal. I set up an automatic telephone call recorder on my home line to record all telephone calls on that line, including when I was out of the house. The illegal bit was that it recorded calls within which I was not a participant. What an ear-burning revelation that was!
Unplanned Escape
In 2003 my father died and left some money to me. Two months later, a new-found friend in Brazil contacted me out of a keen interest in some articles I had written and published on my web site. After considerable correspondence by email, my Brazilian friend effectively offered me a way of escape, which I took. As if subconsciously guided by some unseen hand, I left for Brazil on 23 June 2004. My Brazilian friend became my new life companion and agreed to support me completely.
Her support has been crucial in that, all I have as reward for all my effort of trying to work hard and care for my family in the United Kingdom is an absolute sum total of £92.49 a week State Pension for the rest of my life. This is not inflation protected. It will thus halve its buying power every decade or so. I leave this measly pittance entirely in a UK bank to meet my expenses during my visits to see my children in the UK once every 5 years or so.
Despite having lived under such a torturous workload for over 37 years, to the extent that I was on the point of suicide, I was, nonetheless officially regarded as the bad husband who had "abandoned" his wife.
The diagram below maps my wife's 7 devastating relapses against my career path from 1967, when we got married, until when I left the United Kingdom in 2004.

Since then, to this time of writing in June 2023, my wife has never suffered another relapse. That's 23 years without a relapse. Some assert that, therefore, this must be because I am no longer there causing them. If so, then my exit was all for the best.
Subsequent History
Naturally, after leaving the UK in 2004, I kept in regular communication with my 3 children by email, Skype and Signal. My daughter went to live in Scotland where she gained a master's degree, a management job in a quango that promotes sustainable transport and got married. My younger son emigrated to Canada, became a Canadian citizen and works for the Canadian government. He got married and has 2 children. My elder son was given sheltered accommodation close to where his mother lives in South East England. This was in response to a request I made to his Assertive Outreach Team that he be not forced into the default of living with his mother. Nonetheless, he did end up having to do a lot for her.
My elder son suffered his third relapse in 2016. It comprised just over 9 months of accelerating mayhem that had to be contained by his family and the police, with the usual cack-handed non-intervention by the medical authorities before he was finally sectioned and taken into hospital. This was particularly difficult as my daughter, on top of her demanding job, had to coordinate and manage the whole crisis from over 600km distance. As a result, my daughter decided that the only practical option was to move both her mother and her brother to Edinburgh where they would be close enough to manage any future crises. For my daughter to be saddled with the burden that I had endured for 37 years was the last thing I could have wished for. But it happened. She completed the move in 2021.
But the situation was not good. With the cost of the move, there was no option but for him to live with his mother. Although he has learning difficulties and is utterly incapable of work, the DSS declared him fit for work [brownie points for saving tax-payers' money]. That is, until one day he had a crisis at the Jobcentre itself, whereupon the official dull brains actually managed to perceive that there was a problem. So they made him his mother's carer for which he received "carer's allowance". With the suppressive effects of his medication and his mother's constant torrent of demands, this all became too much for him. He disappeared. He was found living on the street and, clearly in a disturbed state, he was taken into a homeless hostel by the police. From there he was finally "sectioned" and admitted to mental hospital.
It is at this stage that I entered into intense collaboration with my daughter to document, exhaustively but in a digestible form, the history of my elder son's and his mother's mental illnesses. This was to be able to supply my son's psychiatric ward doctor with the best possible briefing.
An Intense Analysis
This exercise revealed to me something, the pivotal significance of which, in my 57 years experience of this phenomenon, I had not noticed before. Both my wife and my son exhibited certain symptoms such as distorted perception, irrational behaviour, anxiety and paranoia only during a relapse. Whereas, on the other hand, they both seemed to subscribe to an abnormal world-view, and exhibited some disruptive character traits that were always present.
In the past, I had been too close to it to see it. That is why I was always incensed and deeply offended when people, completely independently, referred to my wife variously as "the princess", "a lady of leisure", "one of life's passengers". She only ever had one job, which lasted a fortnight, after which she was sacked for lack of productivity and disrupting the work of others. She saw work as social entertainment. In fact, I remember one day when I arrived home tired from work, she railed at me saying "I want to be entertained! What are you going to do about it?" She said that she had been at home alone all day, totally neglected by her husband.
She told people that I was never there: that I was off gallivanting around. People understood from this that I spent my evenings and nights drinking and clubbing with friends. In fact, "never there" meant that I was away every day from 8:30 to 5:30 at work. Work was "having a good time with friends". It is from this that I deduced that she lived in a Period drama world in which a husband's purpose was to have the private means necessary so that he could furnish a very comfortable life-style for his wife and spend all his prime time attending and entertaining her. She had no conception of modern work-a-day life. My son is the same, although to a much lesser extent.
So had my wife been lying when, over the previous 37 years, she had been saying all these terrible things about me to her friends, relatives, her church members, the NHS and the DSS? In the context of a normal world-view, the answer is "yes". People were receiving from her a description of me that was a pure pack of evil, damaging heinous lies. However, in the context of her own 'Period Drama' world-view, she was giving true account. Was this 'Princess' world-view of her own making? Or was it just the way her brain was wired? Was she bad as well as mad? Or was she a victim of socio-biology? I don't know.
What I do know, however, is that what was conveyed caused unbearable and irreparable damage to my life. I was alone. The staff of the medical and social services ostracised me with their disapproving sideways looks. My wife's church members who came to visit her at home kept at arm's length, obviously regarding me as an evil person. Her extended family, who had always regarded me as something the cat brought in anyway, undermined all my efforts to care for my wife at every turn, including conspiring with the medical staff. The only people who saw the reality and gave me any official help were, respectively, a few local neighbours and members of the local police, three of whom lived within our 15-house close.
I could see clearly that my whole personal predicament was entirely society's fault. Family, friends, her church membership, medical staff, social services staff had all taken what my wife had been saying about me at face value without verification or qualification. None of them had had the guts to confront me with it [except for the one church minister I mentioned, whose railings I didn't even understand]. I didn't even know that anything was being said. I was in the dark. All I saw and felt was a nebulous barrage of personal disapproval. As a result, I felt isolated and suicidal. But at that point I decided that I didn't deserve this and that I was simply not going to let society do this to me. By way of defence, I developed an intense and impervious contempt for British society and its institutions.
It was this alone that kept me alive.
My wife's and son's world-views are different from, and incompatible with, the real world. The real world does not behave or respond in the way they think it ought to. Things simply don't compute. Reality cannot be reconciled to perception. This inevitably precipitates a relapse. Thus the mental relapse is not the prime mover. It is a collateral effect of a permanent view of reality which is incompatible with what is really out there, namely, a society that is based upon the structure and principles of free-market capitalism.
In some medical jurisdictions, the state of mind that my wife and elder son have is referred to as a personality disorder. In others it is referred to as a mental illness with permanent symptoms. These different views arise from differences in approach to providing treatment, which are both quite different from taking a pragmatic scientific view of an observed phenomenon.
The basis of my 'scientific' view would have to start with human society as a natural complex-dynamical system with its bell-curve spread of inherent naturally-occurring personality types. In this view, the personality type corresponding to what modern-day society classifies as Entitlement Personality 'Disorder' would be but one of the less numerous personality types 'located' somewhere towards the right-hand edge of the bell-curve. Notwithstanding, this, together with all other personality types [or rather 'traits'] would be present to varying degrees in everybody throughout the whole spread [or spectrum] of human society.
Here I am viewing human society as an idyllic 'confederation' of natural anthropological communities: not the city-based post-industrial juxtapositions of the billions of essentially isolated individuals we have today.
So 'entitlement' seems to be a natural inherent personality trait that is present in all of us. It is just that some people react more strongly to its being taken away from them than do others. And it has a sound systemic basis within the natural order.
Whatever our respective positions within the modern socio-economic order, we all arrived on this planet with nothing. We brought nothing with us to contribute. Likewise, we will all take nothing with us when we leave. But each self resides within a human mind, which is accommodated within a physical brain, which is sustained by a physical body, which is an integral and dependent component of Gaia [the Earth's biosphere]. So to question whether or not each of us is entitled to a proportional share [through a self-evident inalienable right of inheritance] of the planet's resources as the necessary means of turning his labour into his needs of life is like questioning whether or not the kidney is entitled to its blood supply. The question is neither moral nor political: it is purely systemic.
Consequently, the right of entitlement is natural to the human niche within the natural order. So the unusually strong reaction of some to being forcibly deprived, by an unnatural socio-economic order, of that to which they are naturally entitled, is, ipso facto, neither a disorder nor an illness. On the contrary, it is the wholly unnatural socio-economic order of modern free-market capitalism that is causing such over-reactions [plus inexcusable poverty and disparity] by enforcing its incompatible man-made laws upon, and thereby disrupting the proper functioning of, a natural complex-dynamical system.
Crime and Punishment
My police neighbours and their colleagues were often morally apologetic when my wife relapsed. This was because, although they could see that the situation was extremely grave, her behaviour and actions couldn't be formally construed as crimes. So they were powerless to intervene, except in so far as to restore 'public order', which was somewhat of a nebulous notion in this context.
Furthermore, from my entire experience over my 37 years with her, I don't think, in all honesty, that my wife deliberately, wilfully or mindfully constructed her Princess world-view. I think it was just, or became, hard-wired 'into her brain' so to speak. It's possible that the process of constructing her abnormal world-view were triggered or somehow steered by her early life or up-bringing.
One can't simply say that, "Well, none of her siblings ended up this way, so it can't have been her formative situation that generated her Princess personality disorder". On the contrary, the complex-dynamical nature of human society, at all levels, ensures that the niche of experience for each individual — even among siblings — is unique and that the characteristic differences between adjacent niches can be absolutely vast.
So her particular niche within her family and formative society could have at least influenced how her personality was developed. Notwithstanding, I feel quite sure that it must have been largely genetic.
So is she to blame? If indeed she were wilfully pursuing the demands of a Princess personality while in reality perceiving the world the way most other people do, fully aware of the devastating effects her behaviour was inflicting upon her husband and children, then yes, she would be to blame. Consequently, one could argue that she should therefore be punished for what she inflicted on her husband and children.
But somehow, I don't think this was the case. I think she really saw her place in the world as a Princess, or more precisely, as being treated and served the way a princess is treated and served as a de facto normality that it wouldn't even occur to her to question. So she can't be to blame. Therefore, she should not be punished.
It alludes to the age old polemic about the psychopathic serial killer. Is he culpable simply for the way his brain is wired? Should he be hospitalised, imprisoned or executed? It depends on the moral reason. If he mindfully kills while knowing that it is wrong to take human life, then he is to blame and should be punished. On the other hand, if he kills simply because to do so seems normal and natural to him without wilful intent to do something against his natural conscience, then he should not be punished because he's not to blame. But what action, if any, should society take against him? Perhaps he should be hospitalised, imprisoned or executed: not as a punishment but simply as a practical way of protecting and preserving the lives of his possible future victims.
Conclusion
I do not therefore blame my wife for her personality disorder. Nevertheless, her way of being and her behaviour did effectively ruin my life and career, causing serious detriment to our children. Consequently, leaving her — in fact, leaving the country — was a justified act of self-preservation for me once our children had grown up.
Notwithstanding, I do blame society for its arrogant and impervious denial that all the torture we suffered wasn't taking place, just because the quacks couldn't see it. In other words, by deeming or assuming without basis that I, as a first hand observer and sufferer was a perpetual and incorrigible liar against the 'better' judgement of professionals who saw her rarely and had no prolonged exposure to anybody like my wife in a long unmedicated state of relapse.
As her carer, with 24/7 exposure to the situation, I could not only see, but also experience and suffer the devastating effects of her blindingly obvious entitlement personality disorder and the sporadic schizophrenic relapses that the disorder precipitated. Yet neither a general practitioner nor even a specialist like a psychiatrist or community psychiatric nurses ever diagnosed or admitted to there being anything to diagnose until the police eventually had to call them out in the event of a publicly disruptive total relapse.
Whether or not society be morally obliged to benignly accommodate all
naturally existing human personality-types is, of course, a separate issue. I think society is so obliged. But this obligation will never be recognised because society itself has an acute personality disorder of its own. From the distance that I can now view it, it is painfully obvious to me that the British Zeitgeist is — by the collective will and intent of the voting majority — psychopathic. Many generations and perhaps a painful social revolution [as preluded on 06 August 2011] will be required to change it. Perhaps, one day, a violent and bloody social revolution will indeed be its just and well deserved punishment.
I think it is all so shameful, when one considers that under a slightly changed social order, all this suffering, deprivation and hardship simply would not happen. Within a community-based socio-economy, governed by a benign complex-dynamical protocol, the burden of mental illness, like everything else, would be shared not only economically, but also socially and spiritually on a day-to-day basis.
Parent Document | ©May 1998, Dec 2014, Nov 2024 Robert John Morton
 Their blindness to this hardship would be excusable but for one thing; namely, that there is a source of insight into the fact that this hardship exists. That source is the patient's family. What is inexcusable is that this source is ignored or, at best, regarded as having insignificant credibility. The result is the continued non-recognition of this hardship. But sadly, official non-recognition does not make the problem go away. I wish it did. If this professional non-recognition merely resulted in a neutral situation in which the patient's family received no help during a relapse, this would at least be survivable. But it does not. On the contrary, it has created
Their blindness to this hardship would be excusable but for one thing; namely, that there is a source of insight into the fact that this hardship exists. That source is the patient's family. What is inexcusable is that this source is ignored or, at best, regarded as having insignificant credibility. The result is the continued non-recognition of this hardship. But sadly, official non-recognition does not make the problem go away. I wish it did. If this professional non-recognition merely resulted in a neutral situation in which the patient's family received no help during a relapse, this would at least be survivable. But it does not. On the contrary, it has created 